Tag nursing homes
Last fall, a report by UMass Boston researchers showed that Medicaid reimbursements fall short of covering the actual costs of nursing home care for Medicaid residents. That research will now go a step further and try to examine how closely Medicaid payment-to-cost ratios affect outcomes in nursing homes.
For each dollar a nursing home spends providing daily care to a Medicaid recipient, the average nursing home receives just 82 cents in reimbursement. This was the top-level finding of a study published this week, led by multiple researchers, including… Continue Reading →
In 2022, the Moving Forward Nursing Home Quality Coalition asked Marc Cohen to co-lead one of its seven committees created as part of a two-year national initiative to improve nursing home quality. Cohen, co-director of the LeadingAge LTSS Center @UMass… Continue Reading →
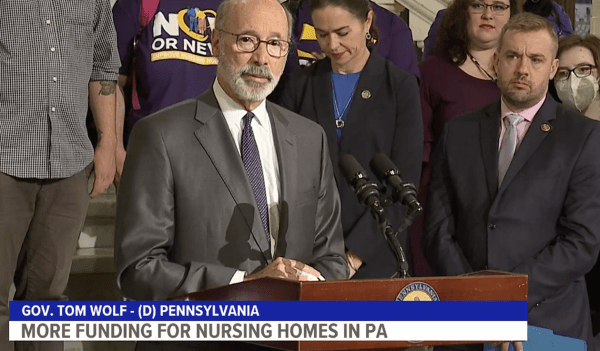
In July 2022, Pennsylvania Governor Tom Wolf and the state’s legislature reached an agreement to boost staffing levels at nursing home facilities. The state will distribute nearly $300 million to nursing homes, representing a roughly 20 percent increase in Medicaid… Continue Reading →
Do Medicaid reimbursement rates to nursing homes cover the costs of the services these facilities provide? That’s the basic question that UMass Boston gerontology researchers will work to answer over the next year. “It’s a common claim that Medicaid reimbursements… Continue Reading →
Jo Owens became a nursing home aide in Canada out of a need for money, and came away with her calling. And from that experience, the pain and the human glory, came her debut novel A Funny Kind of Paradise,… Continue Reading →
I write to announce that Len Fishman, after serving seven years as director of the Gerontology Institute at the McCormack Graduate School of Policy and Global Studies, will be retiring on August 31. A nationally recognized leader in health care… Continue Reading →
Journal of Aging and Social Policy special edition examines scope, impact and lessons drawn from Covid-19 for older adults A special double-issue of the Journal of Aging and Social Policy (JASP) that focused on Covid-19 has been released as a book…. Continue Reading →
UMass Boston gerontologists offered legislators two suggestions for state government in the midst of the COVID-19 pandemic: Help researchers better understand what has happened to older adults and get elder Massachusetts residents prepared for a more challenging future. Gerontology Institute… Continue Reading →
Joanne Lynn is a nationally recognized expert on issues related to palliative and end-of-life care. A geriatrician and hospice physician, she is the author of hundreds of journal articles and many books on issues concerning long-term services and supports. Very… Continue Reading →