Category Management of Aging Services
Glickman Fund supports non-traditional students dedicated to improving older adults’ quality of life
“My life has changed in a direction I never would have seen it gohad I not been an MAS student. I hope to make you all proudas I move forward in my career in aging.”Sophia Casale, MAS ’23, lifestylist, Chelsea… Continue Reading →
The Department of Gerontology at UMass Boston presents five annual awards to deserving graduate students. Four of the awards include a $200 prize to be used for the students’ professional development. Winners of the Capstone Project Award are honored with… Continue Reading →
Dan O’Leary entered the aging services field by happenstance nearly 50 years ago. He was fresh out of school with a bachelor’s degree in political science and a master’s in international relations. Facing a tight job market in the Boston… Continue Reading →
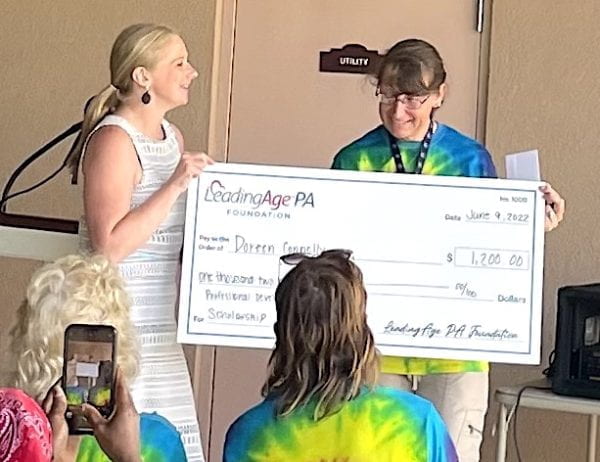
Early in the pandemic in 2020, Doreen Connelly decided she wanted to advance her education past her undergraduate degree. Searching online, she found UMass Boston’s Management of Aging Services graduate certificate program. The five-course program is designed for professionals who… Continue Reading →
Kelly Fitzgerald, PhD ‘08, has been named chair of the NGO Committee on Ageing – Geneva at the United Nations. From her home in Zurich, Switzerland, she has served as the committee’s vice chair over the last eight years, working… Continue Reading →
This article originally appeared on the UMass Boston News web page. We all take different paths in life and, if we’re lucky, we have mentors guiding us along the way. As an undergraduate psychology major, 20-year-old Ellen Birchander was on… Continue Reading →
By Taryn Hojlo Where can I get help? Older adults and caretakers sometimes struggle with that question, unsure how to find aging services and other kinds of assistance they need. Deborah Burton realized there was a thriving demand for those… Continue Reading →
By Taryn Hojlo After years working in management and hospitality, Catherine Williamson was confident she knew how to serve people. For a decade, she had overseen the care of hotel patrons and spa-goers at The Ritz Carlton and Four Seasons…. Continue Reading →
By Taryn Hojlo Two gerontology students researching a multi-generational approach to community senior centers and property tax relief programs for older homeowners have been selected for the 2018 Capstone awards. Students Beth Duggan Rouleau and Norma Strack were selected by… Continue Reading →