Tag
LeadingAge LTSS Center @ UMass Boston
Justice in Aging, a national legal advocacy nonprofit that fights senior poverty through law, has formed an innovative partnership with the Gerontology Institute’s LeadingAge LTSS Center @UMass Boston to support research while enhancing the nonprofit’s capacity to interpret data. The… Continue Reading →
The federal Administration for Community Living (ACL) has awarded Community Catalyst a four-year grant to develop, test, and disseminate new approaches for increasing awareness of family caregivers and building support for their unique concerns. As part of that grant, the… Continue Reading →
A new analysis by the LeadingAge LTSS Center @UMass Boston and the National Council on Aging finds that 80 percent of older Americans—47 million—continue to be unable to sustain a financial shock such as needing to pay for long-term care… Continue Reading →
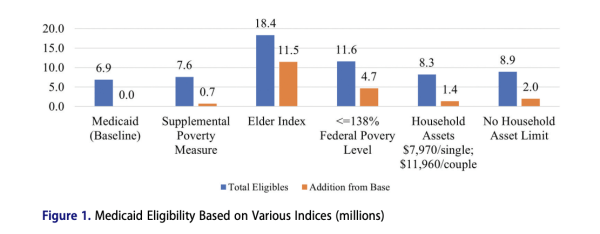
Researchers Marc Cohen and Jane Tavares know how crucial federal programs such as Medicaid health insurance and SNAP food assistance are for the most vulnerable older adults. “Our social safety nets are keeping so many people afloat,” says Tavares, a… Continue Reading →
Researchers at the LeadingAge LTSS Center @UMass Boston are analyzing recent data from the national Health and Retirement Study to update their two previous studies on the relationship between person-centered care and health outcomes. They’re looking to identify any changes… Continue Reading →
By Marc Cohen, Caitlin Coyle, James Hermelbracht, Edward Alan Miller, Jan Mutchler, and Anna-Marie Tabor Older adults are the fastest-growing segment of the American population. In Massachusetts, adults 65 and older will make up nearly a quarter of the Commonwealth’s… Continue Reading →
National strategy roadmap was informed by LeadingAge LTSS Center research It’s been a long time coming, but the needs of family caregivers are starting to receive high-level policy attention. At a White House ceremony on September 21, 2022, the U.S…. Continue Reading →
Marc Cohen, PhD, worked for decades in private industry before joining UMass Boston in 2016. His transition to an academic setting was nearly seamless, he says, because for all those years, “I was a misplaced academic in the corporate world.”… Continue Reading →
Doctoral student Molly Wylie named inaugural fellow for 2022-23. The National Council on Aging (NCOA) and the LeadingAge LTSS Center @UMass Boston have partnered to create an Equity in Aging Research Fellowship. The one-year graduate research position supports both organizations’… Continue Reading →
One-third of people 50 and older report that their health care clinicians rarely or never take into account their care preferences. A person’s race, insurance status, and income level affect the quality of person-centered care they receive, according to a… Continue Reading →