Category
Health
Older adults who smoke heavily have a hard time kicking the habit, even when they receive the most promising cessation treatment. “These are people who started smoking when they were very young, before we knew of all the dangers,” says… Continue Reading →
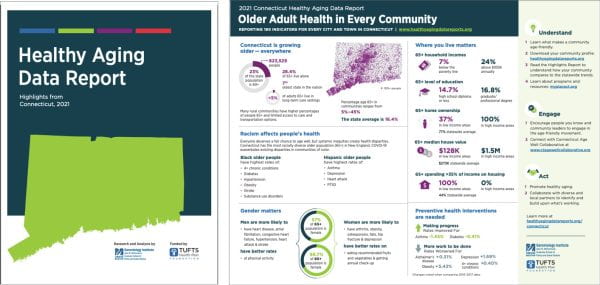
Data for Mississippi and Wyoming contrasts with highly populated New England states For more than a decade, a team of UMass Boston gerontology researchers has been producing detailed reports tracking data related to healthy aging for New England states. The… Continue Reading →
It’s been a busy and productive first year for Jaqueline Contrera Avila, PhD, an assistant professor of gerontology who joined UMass Boston in August 2022. In addition to preparing for and teaching two classes, she has expanded her research on… Continue Reading →
Researchers know that adults with intellectual and developmental disabilities (I/DD) encounter healthcare disparities—fewer doctor’s visits and routine screenings, for example—even though they suffer health complications more frequently than the general population. New research begun by Jeffrey Stokes, PhD, assistant professor… Continue Reading →
A tragic aspect of the pandemic’s prolonged economic downturn – the rising rate of food insecurity in the United States – could impact older, poorer adults and their families for years to come, according to a study by researchers at… Continue Reading →
Jo Owens became a nursing home aide in Canada out of a need for money, and came away with her calling. And from that experience, the pain and the human glory, came her debut novel A Funny Kind of Paradise,… Continue Reading →
Our Marc Cohen and co-author Stuart M. Butler published the following piece this week in Health Affairs, revisiting some of the issues we wrote about earlier while taking a deeper look at this long-standing problem. The Middle Ground for Fixing… Continue Reading →
Marc Cohen and other academics and policy analysts saw the writing on the wall years ago. With roughly 10,000 Americans turning 65 every day, a decades-old medical and financial storm is now on the horizon when it comes to how… Continue Reading →
Internship benefits housing provider and doctoral student while supporting older adult residents When a Boston-based affordable housing developer wanted to survey their residents to better support their health-related needs, they paused. What did they know about approaching older adults to… Continue Reading →
The current financing structure of Pennsylvania nursing homes is not sustainable Nursing homes play a critical role delivering long-term services and supports (LTSS) to older adults and individuals under the age of 65 with disabilities. Despite this, these facilities face… Continue Reading →