
Left to right, associate professor Elizabeth Dugan, professor Nina Silverstein and post-doctoral assistant Chae Man Lee.
A research team at the McCormack Graduate School’s Gerontology Institute published its most recent edition of the Massachusetts Healthy Aging Data Report late in 2018. The report provided detailed information on the health status of older adults across the state. The team, led by associate professor Elizabeth Dugan, also collected a massive amount of local data contained in the report’s 379 separate community profiles.
The Gerontology Institute Blog recently spoke with Dugan and two other team members — professor Nina Silverstein and post-doctoral assistant Chae Man (Jay) Lee — about the report and how it could contribute to the state’s response to the coronavirus pandemic. Here’s what they had to say:
Q: There’s so much information in the Massachusetts Health Aging Data Report. Broadly speaking, how can any of it be useful for those trying to manage the effects of COVID-19 and help older people get though this challenge?
A: The data report provides information that can help state or local policymakers identify areas of high risk for bad outcomes to help prioritize outreach and support. The report contains a wealth of health information on the state, county and local community levels. Much of that data is very relevant to our current situation. But the report also tracks access to care and other important resources for older adults. This information could be particularly helpful for people responsible for allocating support where it is needed most.
Q: What health indicators are tracked in the data report and which ones could be particularly relevant when dealing with the coronavirus?
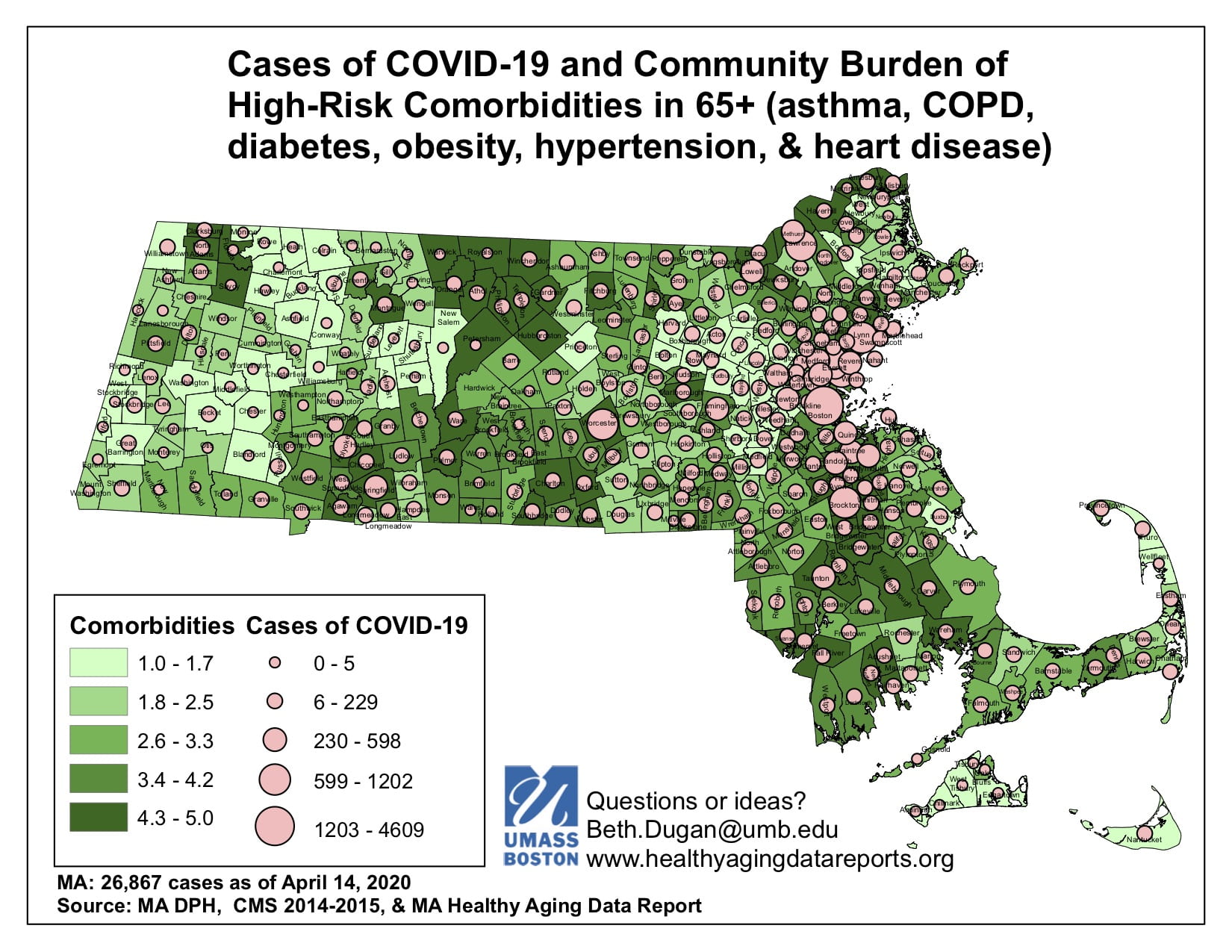
A: Research from China and Italy suggests several specific conditions can heighten the risk for death from the coronavirus. Those are heart disease, lung conditions, hypertension, diabetes and obesity. We track health data that corresponds with each of those conditions to the local level. We’ve combined the community rates on these conditions into a summary measure of risk that highlights communities with more people at higher risk. These communities may be particularly vulnerable to COVID-19 infections.
Q: What did that tell you?
A: Well, as shown on the map (click on map for full-screen view) we see that many communities with the highest rates of the relevant conditions have COVID-19 outbreaks. We are concerned that those communities may end up having high fatal case rates. Now this virus is so transmissible and deadly that maybe anywhere it takes hold will be threatened. But having studied healthy aging in Massachusetts for years, our concern is focused on the communities with high rates of critical co-morbidities. Many are so-called gateway cities with populations who are disadvantaged in terms of the social determinants of health.
Q: You mentioned that the Healthy Aging Data Report also tracks the access to health care for older adults across the state. What does that show and how is it relevant right now?
A: We report access to primary care, hospitals, home health care, and nursing homes. For people who survive COVID-19, post-acute care, rehabilitation, or other supportive service may be needed. The data report helps people to know what is available in their area. Not surprisingly, we see less access in the more rural parts of Massachusetts.
Q: You also track the availability of food – supermarkets and grocery stores in an area, and how far some older people need to travel to get there.
A: Yes, we have identified communities that have poor supermarket access and also communities where people are not eating a healthy diet (fruits and vegetables). These communities may have older residents at risk of food insecurity during normal times, which is even worse during the current crisis.
Q: Your report also looked at health disparities based on race and ethnicity. Much higher coronavirus-related fatality rates among Black and Hispanic populations have been seen in areas across the country. Is there anything in your health data that relates to a heightened COVID-19 risk?
A: We have found that healthy aging varies by where people live, work, and play. There are disparities by race and community type — urban, suburban or rural. The impact of COVID-19 appears to follow the same pattern. We see higher case rates and worse outcomes in communities of color. The availability of testing is still limited despite the best efforts of the state and medical community, so we still are guessing to some extent on how many people have been infected.


Leave a Reply